The National Institutes of Health is beginning a handful of studies to test possible treatments for long COVID, an anxiously awaited step in U.S. efforts against the mysterious condition that afflicts millions.
Monday’s announcement from the NIH’s $1.15 billion RECOVER project comes amid frustration from patients who’ve struggled for months or even years with sometimes-disabling health problems — with no proven treatments and only a smattering of rigorous studies to test potential ones.
“This is a year or two late and smaller in scope than one would hope but nevertheless it’s a step in the right direction,” said Dr. Ziyad Al-Aly of Washington University in St. Louis, who isn’t involved with NIH’s project but whose own research highlighted long COVID’s toll. Getting answers is critical, he added, because “there’s a lot of people out there exploiting patients’ vulnerability” with unproven therapies.
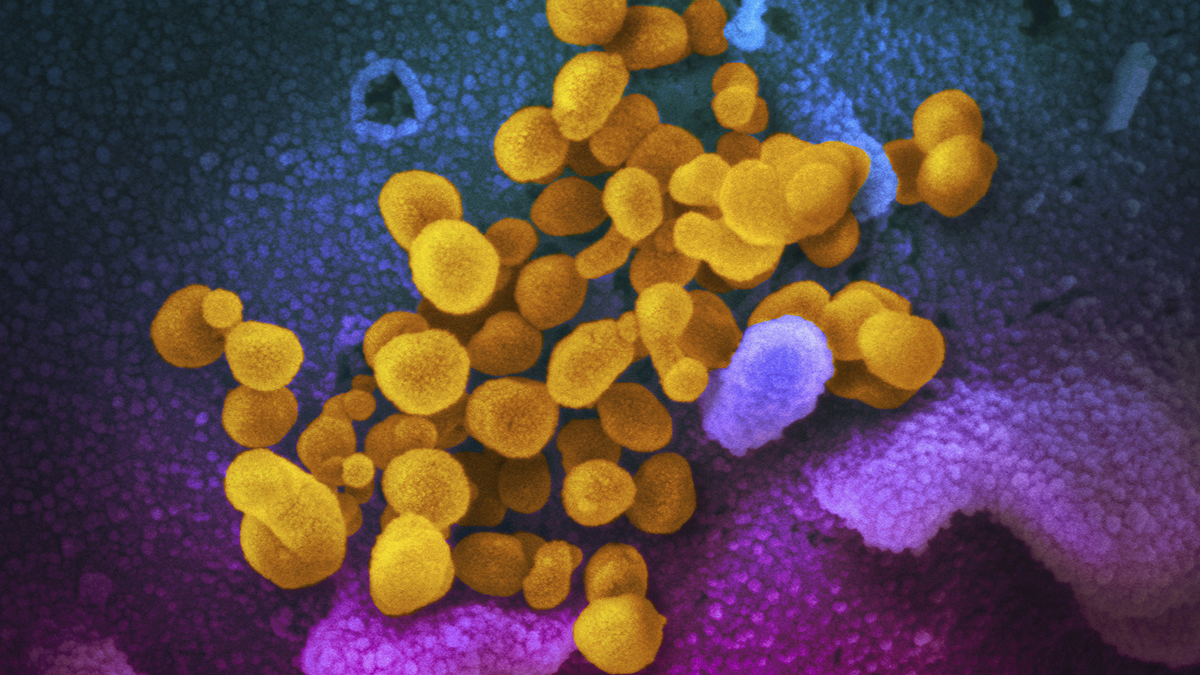
Scientists don’t yet know what causes long COVID, the catchall term for about 200 widely varying symptoms. Between 10% and 30% of people are estimated to have experienced some form of long COVID after recovering from a coronavirus infection, a risk that has dropped somewhat since early in the pandemic.
Get Tri-state area news delivered to your inbox.> Sign up for NBC New York's News Headlines newsletter.
“If I get 10 people, I get 10 answers of what long COVID really is," U.S. Health and Human Services Secretary Xavier Becerra said.
That's why so far the RECOVER initiative has tracked 24,000 patients in observational studies to help define the most common and burdensome symptoms — findings that now are shaping multipronged treatment trials. The first two will look at:
- RECOVER-VITAL: Whether taking up to 25 days of Pfizer's antiviral drug Paxlovid could ease long COVID, because of a theory that some live coronavirus, or its remnants, may hide in the body and trigger the disorder. Normally Paxlovid is used when people first get COVID-19 and for just five days.
- RECOVER-NEURO: Treatments for “brain fog” and other cognitive problems. They include Posit Science Corp.’s BrainHQ cognitive training program, another called PASC-Cognitive Recovery by New York City’s Mount Sinai Health System, and a Soterix Medical device that electrically stimulates brain circuits.
Two additional studies will open in the coming months.
- RECOVER-SLEEP: Will test treatments for sleep problems. A trial for hypersomnia, or excessive daytime sleepiness, will test two wakefulness-promoting drugs compared to a placebo control. A second trial for sleep disturbances, such as problems falling or staying asleep, will test other interventions designed to improve sleep quality to learn if these interventions may help regulate sleep patterns in adults with long COVID.
- RECOVER-AUTONOMIC: Will target problems with the autonomic nervous system — which controls unconscious functions like breathing and heartbeat — including the disorder called POTS. (POTS), a disorder with a number of symptoms including irregular heartbeat, dizziness and fatigue, and will have multiple study arms. The first arm will evaluate a treatment used for immune diseases versus placebo. The second arm will evaluate a drug currently used to treat chronic heart failure in people with an elevated heart rate versus placebo.
A more controversial study of exercise intolerance and fatigue also is planned, with NIH seeking input from some patient groups worried that exercise may do more harm than good for certain long COVID sufferers.
The trials are enrolling 300 to 900 adult participants for now but have the potential to grow. Unlike typical experiments that test one treatment at a time, these more flexible “platform studies” will let NIH add additional potential therapies on a rolling basis.
“We can rapidly pivot,” Dr. Amy Patterson with the NIH explained. A failing treatment can be dropped without ending the entire trial and “if something promising comes on the horizon, we can plug it in.”
The flexibility could be key, according to Dr. Anthony Komaroff, a Harvard researcher who isn’t involved with the NIH program but has long studied a similarly mysterious disorder known as chronic fatigue syndrome or ME/CFS. For example, he said, the Paxlovid study “makes all sorts of sense,” but if a 25-day dose shows only hints of working, researchers could extend the test to a longer course instead of starting from scratch.
Komaroff also said that he understands people's frustration over the wait for these treatment trials, but believes NIH appropriately waited “until some clues came in about the underlying biology," adding: “You’ve got to have targets.”