A common respiratory virus that can make kids (and some adults) severely sick is concerning doctors because it emerged far earlier than usual this year and is already filling up hospital beds across the country.
Pediatric hospital bed capacity is already strained in nearly a half-dozen states because of the atypical influx, doctors say. And with many now conditioned to assume any cold-type ailment is likely COVID or the flu, pediatricians -- and the CDC -- want to be sure parents know about RSV, how to identify symptoms in your child and what to do about them.
Here are a few things they want you to know.
Get Tri-state area news delivered to your inbox.> Sign up for NBC New York's News Headlines newsletter.
What Is RSV? Some Fast Facts
Short for respiratory syncytial virus, RSV is a common ailment that usually causes mild cold-like symptoms, according to the CDC. Most people recover in a week or two, but the virus can be serious, particularly for infants and older adults.
The virus typically peaks in winter, but it started to circulate this summer, which surprised -- and concerned -- doctors, and likely reflects how the COVID pandemic disrupted circulation patterns for conditions like RSV. The CDC says the season usually starts between mid-September and mid-November and peaks in late December to mid-February.
Positive tests start to drop between mid-April and mid-May, typically. Florida has an earlier onset of the RSV season and it lasts longer there as well compared with other parts of America.
RSV is the most common cause of bronchiolitis (inflammation of small airways in the lungs) and pneumonia (lung infection) in kids younger than 1 in the United States.
According to the CDC, each year RSV leads to about:
- 2.1 million doctor visits among kids younger than 5
- 58,000 hospitalizations among kids younger than 5
- 177,000 hospitalizations among adults aged 65 and up
- 14,000 deaths among adults aged 65 and up
- 100 to 300 deaths in children younger than 5
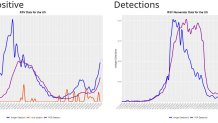
Little comparative data for this season is available thus far, based on testing limitations and other factors, per the CDC. The five-week average for positive RSV PCR tests in New York, for example, has risen weekly since mid-April, when the last season ended. The average for the week ending Oct. 8 is 133.333, up from 41.4 in early August as the CDC began to note earlier-than-usual trends. That compares with a five-week average of 47.333 positive PCR tests in New Jersey ending that Oct. 8 week. Connecticut data is incomplete. See more state-by-state analysis here.
How Is RSV Diagnosed and What Are the Symptoms?
Like COVID, RSV can be diagnosed via antigen or PCR test. The most common diagnostic measure is a mouth swab or blood test that assesses white blood cell count, which viruses affect. In severe cases, additional testing like chest X-rays or CT scans might be needed to evaluate potential lung complications.
Symptoms are similar to both COVID, the common cold and flu. According to the CDC, people typically show symptoms within four to six days after becoming infected. Those may include runny nose, coughing, sneezing, fever, wheezing and a decrease in appetite. Notably, the symptoms usually appear in stages and don't hit all at once.
Almost all kids will have had an RSV infection, diagnosed or not, by their second birthday, according to the CDC. For very young infants, irritability, decreased activity and breathing struggles may be the only identifiable symptoms.
Parents are advised to call their pediatricians if their child is having breathing difficulty, not drinking enough fluids or experiencing worsening symptoms. Dehydration and trouble breathing are more likely to lead to severe cases and hospitalizations. In the worst ones, kids may need to be intubated. In most cases, hospitalizations last a few days.
More Health News
How Is RSV Transmitted -- and What About Treatment?
RSV transmission is also similar to how COVID and cold-like illnesses are spread. This virus spreads when an infected person coughs or sneezes; you get virus droplets from a cough or sneeze in your eyes, nose or mouth; you touch a surface that has the virus on it, like a doorknob, and touch your face without washing your hands; and you have direct contact with the virus, like kissing the face of an infected child.
The contagious period typically lasts three to eight days, but in cases involving some infants or immunocompromised adults, RSV can keep spreading for as long as a month even when patients no longer show symptoms.
Kids are often exposed to RSV outside the home, like in school or childcare centers, and can transmit it to family.
RSV can survive for many hours on hard surfaces like crib rails and tables and typically lives on soft surfaces like tissues and hands for a shorter duration.
You can get RSV at any age, but later-life infections tend to be less severe, the CDC says. People at heightened risk for severe illness from RSV include premature infants, young kids with congenital heart or chronic lung disease, people with weakened immune symptoms and older adults, especially those with underlying heart or lung conditions.
There is no specific treatment for RSV infection, but researchers are working to develop antivirals and vaccines. A drug called palivizumab is available to prevent severe RSV illness in some kids, but the CDC says it can't help cure or treat kids already suffering from severe RSV-related illness and it cannot prevent infection.
What About Symptom Relief and Prevention?
Over-the-counter fever reducers and pain relieves like acetaminophen or ibuprofen can help manage fever and pain, though parents should never give aspirin to their children. Be sure infected people stay hydrated.
Here's what the CDC has to say on prevention, which should sound familiar:
- Cover your coughs and sneezes with a tissue or your upper shirt sleeve, not your hands
- Wash your hands often with soap and water for at least 20 seconds
- Avoid close contact, such as kissing, shaking hands, and sharing cups and eating utensils, with others
- Clean frequently touched surfaces such as doorknobs and mobile devices
When possible, people with cold-like symptoms should avoid interacting with kids at high risk for severe RSV. If they can't, they should adhere to the prevention steps and make sure not to kiss high-risk children while symptomatic.
Parents of high-risk children are advised to take additional precautions, the CDC says. Those include:
- Avoid close contact with sick people
- Wash their hands often with soap and water for at least 20 seconds
- Avoid touching their face with unwashed hands
- Limit the time they spend in child-care centers or other potentially contagious settings, especially during fall, winter, and spring. This may help prevent infection and spread of the virus during the RSV season




