A dangerous and potentially deadly fungal infection is spreading fast, and researchers say our changing climate is partly to blame.
Those experts aren't worried about an apocalypse like the one seen in HBO's "The Last of Us," but there is cause for concern.
You may have seen some of the headlines, as the CDC warns of a deadly fungal infection spreading at an alarming rate.
"The reason this is worrisome is because this is a relatively new fungus," said Dr. Arturo Casadevall, a professor at the Johns Hopkins School of Public Health. He's been studying fungal infections for three decades.
Get Tri-state area news delivered to your inbox.> Sign up for NBC New York's News Headlines newsletter.
"And once it gets into a hospital, into a nursing home or into a health care facility, it is difficult to eradicate."
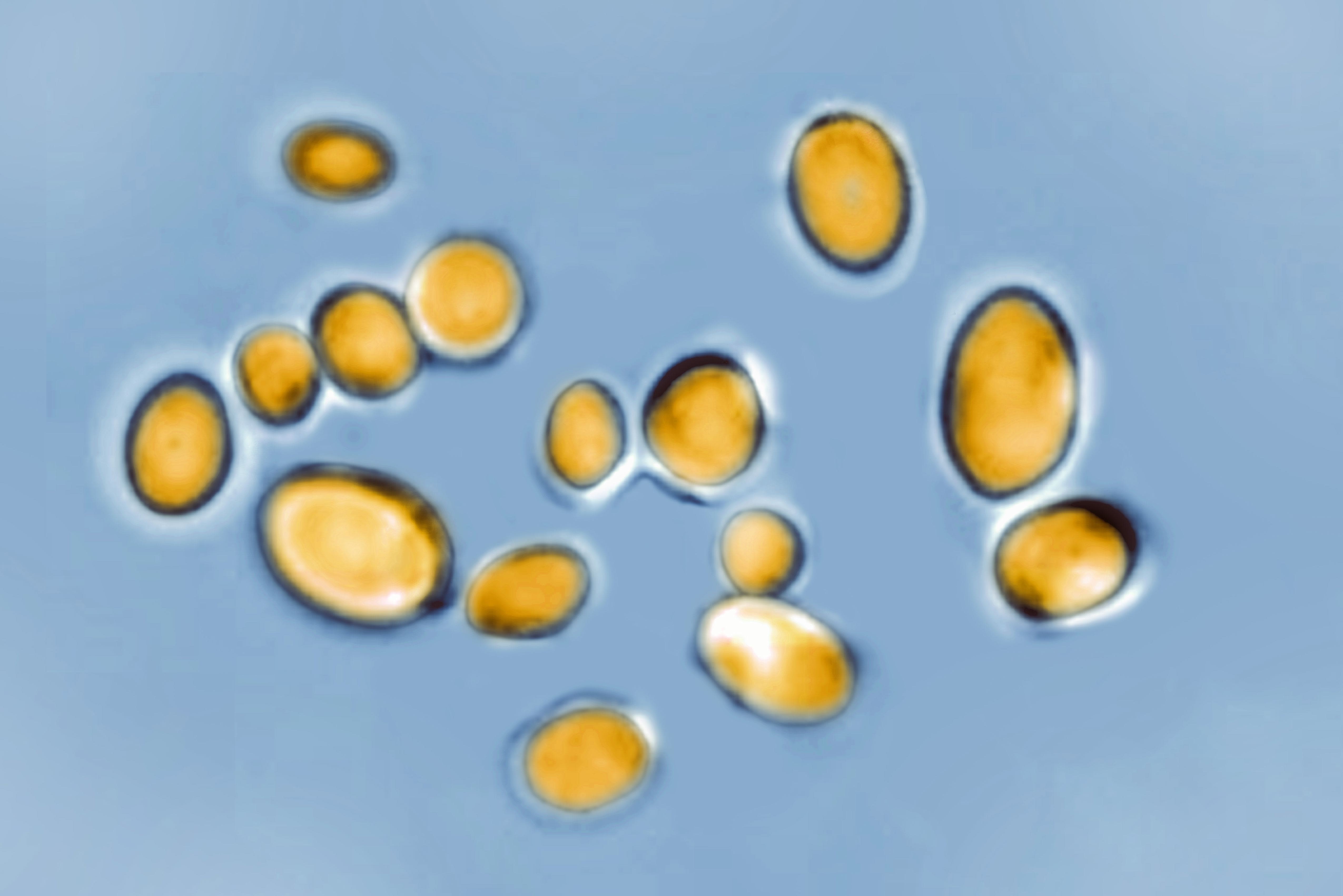
The fungus is called Candida Auris, and it's a drug-resistant fungus that’s been reported in more than half of states in the U.S. -- including Maryland and Virginia.
Casadevall says C. Auris is typically not harmful to healthy people with strong immune systems. But it can be serious, even deadly, among those who are immunocompromised.
"This is a fungus that causes disease primarily in debilitated individuals who are hospitalized or institutionalized in some way," said Casadevall. "The majority of healthy people with immune systems and no medical problems don't really have to worry about Candida Auris."
Despite outbreaks at some hospitals and healthcare facilities, scientists say the situation is not like the zombie apocalypse in "The Last of Us."
"'The Last of Us' is fiction," Casadevall said. "It's fun to watch. But currently, an organism like that doesn't exist. When reporters ask me, 'Is this possible?' My answer is always improbable, but not impossible."
That’s because fungal infections continue to evolve and adapt, thanks to climate change.
"With climate change and global warming, some of the fungi will adapt to higher temperatures," Casadevall said. "And I and some of my colleagues have proposed that Candida Auris is the first example of that."
He says scientists have long known about the impacts of this fungus on frogs and bats. But now that humans are affected, we need to be more aware.
That awareness involves educating people about symptoms, educating hospitals on infection control, and educating researchers so they can develop treatment options, Casadevall said.
"It's not happening like COVID that burst into our consciousness all of a sudden," he said. "It's happening gradually. And this is why vigilance, research, and awareness is the way to protect yourself in the future."
According to Casadevall, the fungus can live on surfaces and on a person’s skin, infecting the bloodstream, heart, or brain.
Symptoms can vary greatly depending on the type of infection, but fever and chills are the most common, CNBC reported in late March. People with weak immune systems, who have diabetes, who take a lot of antibiotics or who are on breathing tubes, feeding tubes and catheters are more likely to be affected.
By getting the word out, hospitals and nursing homes can have measures in place to disinfect contaminated areas and treat the sick. The CDC is also working to find better treatments.
There are already antifungal medications that work, Casadevall said, and once someone is treated and recovers, they're cured.