- Achieving herd immunity with Covid vaccines when the highly infectious delta variant is spreading is "not a possibility," a leading epidemiologist said.
- Herd immunity is achieved when a majority of people in a population are immune to a virus or disease. It's achieved through vaccination or natural infection, leading to reduced transmission.
- Sir Andrew Pollard, head of the Oxford Vaccine Group, described the idea of achieving herd immunity as "mythical."
LONDON — Achieving herd immunity with Covid vaccines when the highly infectious delta variant is spreading is "not a possibility," a leading epidemiologist said.
Experts agree on several reasons why such a goal — where overall immunity in a population is reached and the spread of the virus is stopped — is not likely.
Sir Andrew Pollard, head of the Oxford Vaccine Group, told British lawmakers Tuesday that as Covid vaccines did not stop the spread of the virus entirely — with vaccinated people still able to be infected and transmit the virus — the idea of achieving herd immunity was "mythical."
"I think we are in a situation here with this current variant where herd immunity is not a possibility because it still infects vaccinated individuals," said Pollard, one of the lead researchers in the creation of the AstraZeneca-University of Oxford vaccine.
"And that does mean that anyone who's still unvaccinated, at some point, will meet the virus. That might not be this month or next month, it might be next year, but at some point they will meet the virus and we don't have anything that will stop that transmission."
Get Tri-state area news delivered to your inbox. Sign up for NBC New York's News Headlines newsletter.
Read more: Fully vaccinated people are still getting infected with Covid. Experts explain why
Money Report
What is herd immunity?
Put simply, herd immunity relates to the idea that a high level of immunity to a virus in a population can be achieved by both natural infection (through the forming of antibodies when the body fights a virus) and by vaccination.
The latter method is preferred as vaccines overwhelmingly create immunity without causing illness or adverse health complications, unlike the natural infection route.
The antibodies procured by natural infection and vaccination usually protect against future infection. If enough people in a population are immune this leads to lower rates of prevalence of disease or viruses in a community. If a virus has less opportunity to spread and infect, it can be greatly controlled or even eradicated.
With herd immunity, those who are not vaccinated (whether through choice or because they cannot be immunized at a given point — newborn babies, for example) are protected by the overall level of immunity present in a population.
Mass, successful vaccination programs have meant deadly, contagious viruses and diseases such as polio, tuberculosis and measles have been largely eradicated in parts of the world or greatly suppressed by vaccination programs and the herd immunity they foster.
Pollard noted on Tuesday that Covid, and the current virulent delta variant, are different. "The problem with this virus is [it is] not measles. If 95% of people were vaccinated against measles, the virus cannot transmit in the population," he told the U.K.'s All-Party Parliamentary Group on the coronavirus.
Pollard said that while Covid vaccines might slow the spread of the virus — because fully vaccinated but infected people appeared, in studies, to shed less virus, giving the virus less opportunity to spread — new variants were likely to emerge that would also spread.
"I suspect that what the virus will throw up next is a variant which is perhaps even better at transmitting among vaccinated populations and so that's even more of a reason not to be making a vaccine program around herd immunity."
People who are fully vaccinated are highly protected against severe infection, hospitalization and death caused by the virus. New research from the U.K. released Friday also showed that double vaccinated people were three times less likely than unvaccinated people to test positive for the coronavirus. The research, led by Imperial College London, also suggested that fully vaccinated people may be less likely than unvaccinated people to pass the virus on to others.
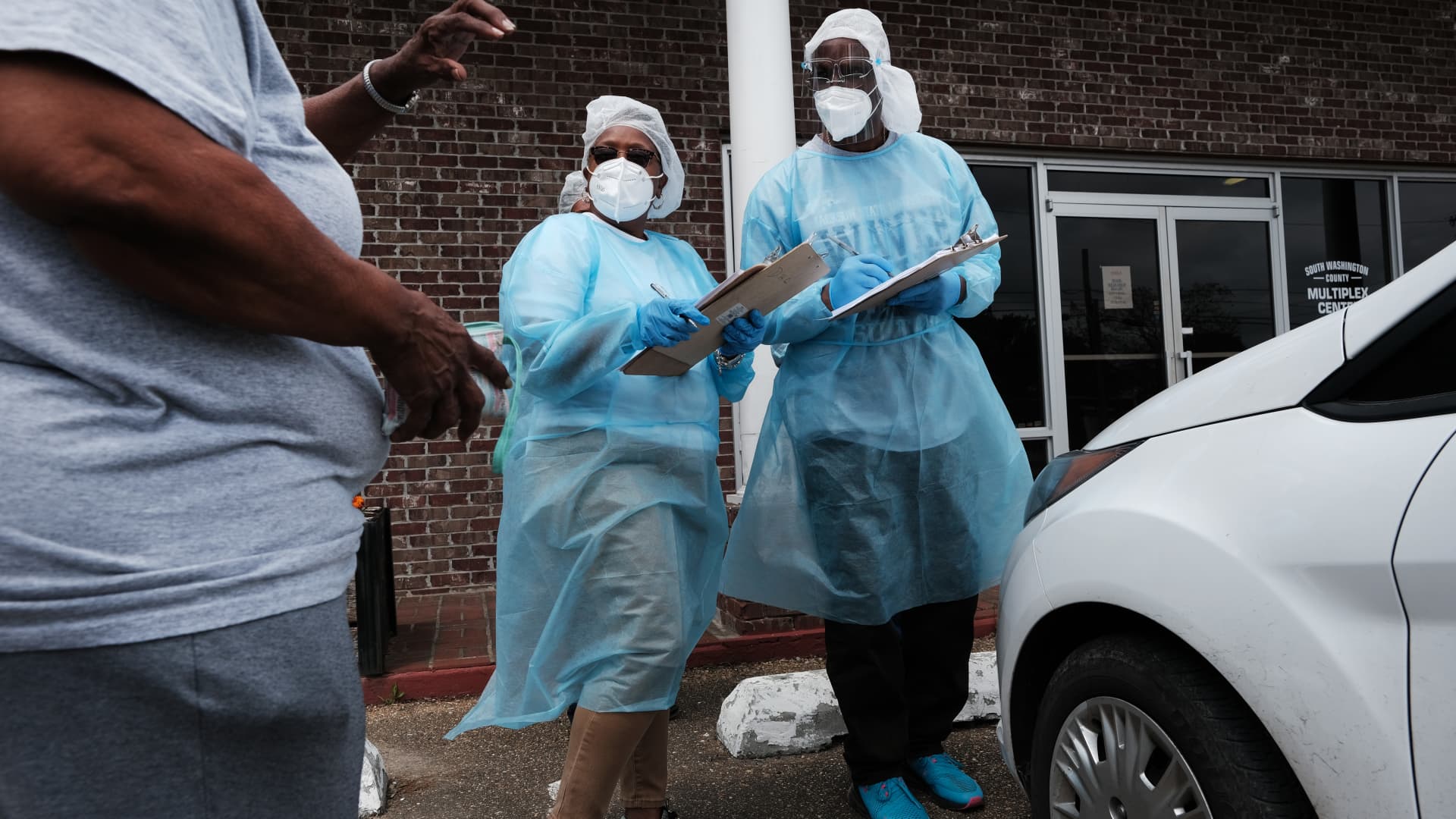
Experts are calling on all unvaccinated individuals to come forward, but issues are emerging in some countries in Europe and the U.S. with younger adults not taking up the vaccine.
Dr. Andrew Freedman, reader in infectious disease at Cardiff Medical School, told CNBC on Thursday that he agreed with Pollard's assessment that herd immunity was unlikely.
"The delta variant is highly transmissible meaning that the proportion of people needing to be fully vaccinated for herd immunity is probably not achievable," he said. "The vaccines provide very effective protection against severe disease/hospitalisation/death but are less effective in preventing infection, mild disease and transmission, especially for the delta variant."
In countries like the U.K., herd immunity was also unlikely due to the large pool of unvaccinated adolescents and children — some of whom would have immunity following natural infection but most would not, Freedman said.
"However, even without complete 'herd immunity,' the higher the proportion of the population fully immunised, the lower the incidence of infection in the community," he said.
Problems with herd immunity
When the coronavirus pandemic started to sweep around the world in 2020, a number of governments, such as those in Sweden and the U.K., appeared ready to pin their hopes on the concept of "herd immunity," willing to let the virus spread among their populations so that natural immunity could build.
The approach was quickly abandoned by the U.K., however, as it quickly became apparent just how deadly and destructive Covid could be, with thousands of infections leading to hospitalizations and deaths that threatened to overwhelm the health system.
Achieving herd immunity when it comes to Covid is seen to be much harder for several other reasons, including uneven vaccine rollouts, vaccine hesitancy and the mutation of the virus, with new variants threatening (but not yet undermining) Covid vaccine efficacy.
Read more: As Covid mutations spread, will herd immunity ever be possible?
In addition, experts don't yet know how long immunity to Covid lasts, although there is clinical evidence that immunity against the virus wanes over time.
Studies show that the Covid vaccines in use in Europe and the U.S. are still highly effective at preventing severe infections, hospitalizations and deaths. While there is evidence of so-called breakthrough Covid cases among fully vaccinated people, these cases are rare and tend to be milder.
Danny Altmann, professor of immunology at Imperial College London, told CNBC that he also agreed with Pollard and that the herd immunity mathematical model could not easily be applied to an "unprecedented" virus like Covid that was still little understood with diverging, globally circulating variants emerging.
"The whole herd immunity thing was one of those bits of medical textbook-speak that was adopted early on by policy advisors, then the press, then the public and has throughout been contorted and over-simplified," he said Thursday.
What was important, Altmann said, was that "the more people on the globe effectively vaccinated, the fewer viral copies we'll have on the planet, thus the less spread and fewer lungs in which for virus to mutate and spread the next wave of variants."